View resources
Key points
- Inhaled foreign bodies can lead to serious complications including death.
- Seek urgent senior emergency/paediatric advice for a child with airway concerns. Consider contacting other available senior resources onsite including anaesthetics, critical care or ENT.
- A bronchoscopy is recommended for diagnostic or therapeutic purposes for a child with a history of foreign body inhalation and abnormal findings on physical and/or radiological examination or ongoing or unexplained respiratory symptoms.
Purpose
This document provides clinical guidance for all staff involved in the care and management of a child presenting to an Emergency Department (ED) in Queensland with a suspected or confirmed inhaled foreign body.
This guideline has been developed by senior ED clinicians and Paediatricians across Queensland, with input from ENT and Respiratory, Queensland Children’s Hospital, Brisbane. It has been endorsed for use across Queensland by the Queensland Emergency Care of Children Working Group in partnership with the Queensland Emergency Department Strategic Advisory Panel and the Healthcare Improvement Unit, Clinical Excellence Queensland.
Introduction
Inhaled foreign bodies are more common in the following children:
- aged one to three years due to oral exploration and immature dentition
- children with older siblings
- older children with neurological conditions or depressed conscious level
Common inhaled foreign bodies in younger children include peanuts, seeds and beans. Older children tend to inhale non-food items such as coins, paperclips and pen caps.1
Inhalation can result in pharyngeal/ laryngeal lodgement or passage down the respiratory tract. Most inhaled foreign bodies lodge in the bronchi with a predisposition for the right main bronchus. Laryngo- tracheal foreign bodies are less common but are associated with an increased risk of fatality. Large items and those with sharp edges are most likely to become impacted in the larynx.
Inhaled foreign bodies that are round and non-compressible with smooth, slippery surfaces pose most risk of complete airway obstruction. Deflated/ broken balloons are the foreign body most likely to result in death.
Later sequelae include atelectasis, pneumonia, granuloma formation, abscesses, broncho-oesophgeal fistulae and bronchiectasis. The risk of these increases with the length of time between aspiration and diagnosis.1
Assessment
Button batteries require immediate removal to prevent necrosis of surrounding tissue.
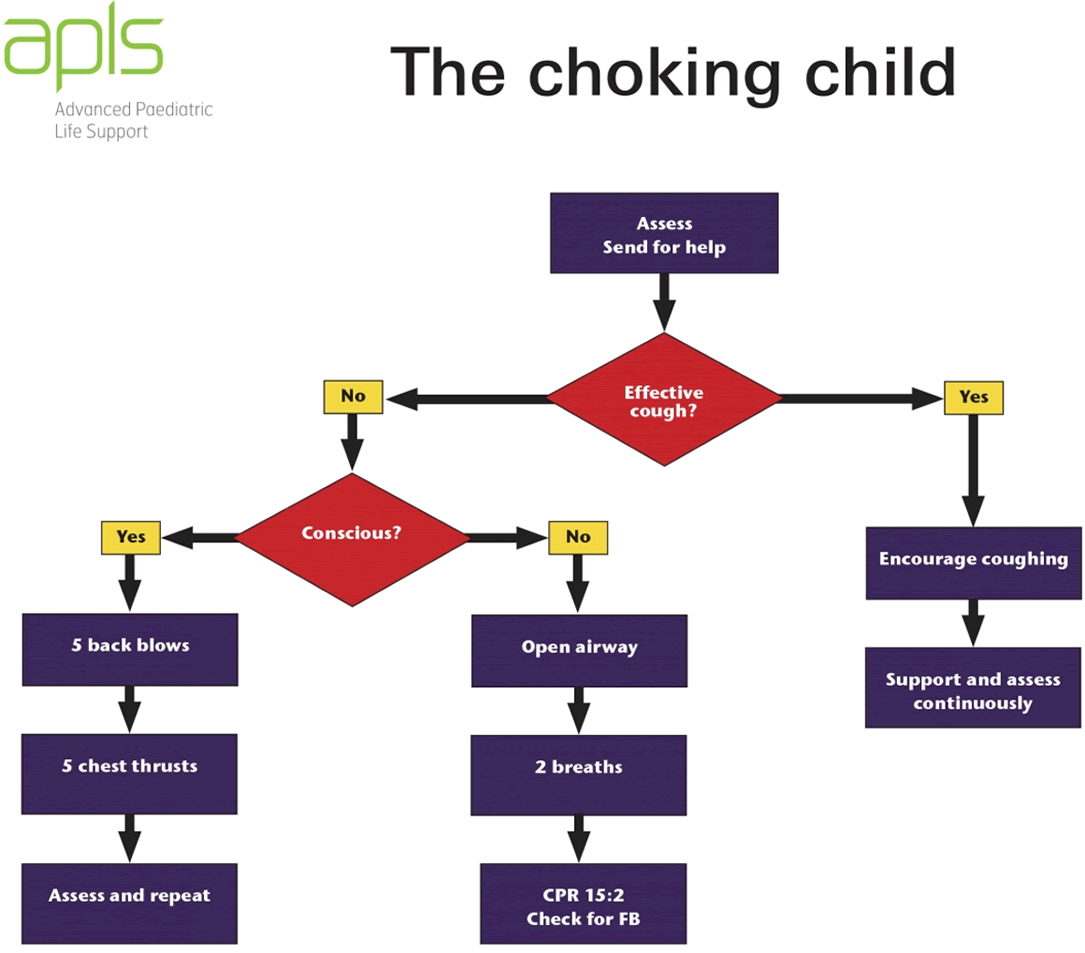
Conduct an initial assessment of airway, breathing and circulation in line with APLS guidelines2 and undertake appropriate action.
When to suspect an inhaled foreign body
A history of aspiration may be reported by child or caregiver however children with inhaled foreign bodies may be asymptomatic for weeks or months with only 85% being confirmed on history.1 Maintain a high level of suspicion of an inhaled foreign body in children who present with the following symptoms, particularly if onset is sudden.1,3-5
- stridor
- cyanotic episode
- drooling
- choking/ gagging followed by coughing
- haemoptysis
- unilateral wheeze or diminished breath sounds
Consider the possibility of foreign body inhalation in a child with prolonged or recurrent respiratory symptoms particularly if failing to respond to standard medical therapy. In some cases, inhaled foreign bodies can precipitate a generalised wheeze that responds partially to bronchodilators with residual focal areas of wheeze.
History
History taking should include questioning on:
- choking history:
- especially in previously healthy child with a sudden onset of cough, dyspnoea or cyanosis
- choking episodes can last from seconds to minutes, are usually self-limited and may be followed by a symptom free period
- information may not be spontaneously offered by caregivers and may require direct and repeated questioning
- the size, shape and nature of the potential foreign body to determine:
- likely site of impaction
- risk of airway obstruction
- likelihood of radio-opacity
Examination
Systematic physical examination and cardio-respiratory monitoring should be undertaken with initial focus on airway and breathing.
Signs consistent with upper airway (laryngotracheal) foreign bodies include:
- voice change
- barking cough
- stridor
- acute respiratory distress.
Signs of oesophageal perforation associated with laryngeal or large penetrating foreign bodies include:
- erythema on the neck
- neck swelling
- crepitus over neck and upper chest.
Signs of lower airway foreign body include:
- cough
- regional variation in aeration
- focal monophonic wheeze
- dyspnoea
- asymmetrical chest movement
- tracheal deviation.
Fever should raise suspicion of secondary tracheitis or pneumonia following aspiration.
| Croup |
| Asthma |
| Respiratory tract infection |
| Pneumothorax |
Investigations
Chest X-rays are recommended for all children with suspected lower airway foreign body. If an upper airway foreign body is suspected only consider X-rays in a child with a stable airway.
X-rays should be reviewed for radio-opaque foreign bodies, lobar collapse, unilateral hyperinflation and mediastinal shift as well as signs of perforation, pneumothorax, and pneumomediastinum.5 In delayed diagnosis of inhaled foreign body, plain films can show late manifestations such as pneumonia, abscesses and bronchiectasis.1
Normal plain film radiography cannot exclude foreign body inhalation as up to 35% of cases have normal images in the first 24 hours. Expiratory and chest decubitus films may increase sensitivity but are difficult to perform in children due to limited cooperation.
Lateral soft tissue neck X-rays are a useful tool for upper aerodigestive tract foreign bodies and can show widened pre-vertebral shadow and loss of lordosis in addition to radio-opaque foreign bodies. They are recommended to better define whether a proximal foreign body is in the airway or gastrointestinal tract.
Management
Refer to flowchart [PDF 209.81 KB] for a summary of the emergency management for a child with an inhaled foreign body:
Urgent referral to ENT team (onsite or via Retrieval Services Queensland (RSQ)) is required for children with:
- signs and symptoms of upper airway obstruction
- respiratory distress
- abnormal vital signs
- other signs and symptoms of concern to treating clinician
Prompt referral to ENT via local practices is required for stable patients requiring diagnostic or therapeutic bronchoscopy.
All patients with inhaled foreign bodies should be referred to ENT initially who will contact the respiratory team at their discretion.
Upper airway foreign body
Seek immediate senior assistance onsite (emergency/paediatric/anaesthetics/critical care/ ENT) in a child with airway concerns or inhaled button battery.
Evaluate and manage airway compromise in accordance with APLS guidelines.2
Supportive management is recommended initially in a child with no immediate airway concerns. Nurse the child in a position of comfort with cardiorespiratory monitoring and supplemental oxygen as required.
Nebulised adrenaline is not recommended due to the risk of dilation permitting distal movement of the foreign body resulting in complete airway obstruction.1
Foreign body removal with Magill forceps under direct visualisation must only be performed in controlled environments in a setting with skills and resources for advanced airway management.1
All children with suspected foreign body inhalation should be kept nil by mouth pending investigations and consultation with subspecialty teams, if required.
Apply topical amethocaine (or equivalent) in preparation for IV cannulation.
Avoid potentially distressing procedures in a child with upper airway compromise.
Lower airway foreign body
Bronchoscopy is recommended for diagnostic and/ or therapeutic purposes for the following children:
- history of foreign body inhalation and either:
- abnormal findings on physical or radiological examination or
- ongoing symptoms despite normal physical and radiological findings
- unexplained atypical/prolonged respiratory symptoms that have failed to respond standard medical therapy
Bronchoscopy is not recommended on initial presentation for children with a clear history of choking and normal physical and radiological findings as the risk of bronchoscopy is considered to exceed the risk of a retained inhaled foreign body. A bronchoscopy may be indicated if these children develop otherwise unexplained respiratory symptoms within a month of the incident.
Seek ENT advice in a child who presents with otherwise unexplained respiratory symptoms within a week of a choking episode.
Seek Paediatric Respiratory advice (if available locally), or Paediatric/ENT service as per local practice in a child who presents with otherwise unexplained respiratory symptoms more than a week after a choking episode.
Escalation and advice outside of ED
Clinicians can contact the services below if escalation of care outside of senior clinicians within the ED is needed, as per local practices. Transfer is recommended if the child requires a higher level of care.
Critically unwell or rapidly deteriorating child
| Service | Reason for contact | Contact |
|---|---|---|
| Immediate assistance with airway | For onsite help with management of airway/intubation anticipating a difficult airway. |
The most senior resources available onsite at the time as per local practices.
Options may include:
|
| ENT |
For urgent advice/assistance in the following children with an inhaled foreign body:
|
Onsite or via Retrieval Services Queensland (RSQ).
If no onsite service contact RSQ on 1300 799 127:
RSQ (access via QH intranet) Notify early of children potentially requiring transfer. In the event of retrieval, inform your local Paediatric service. |
| Paediatric Surgery | For urgent management of child with suspected oesophageal perforation associated with laryngeal or large penetrating foreign bodies. | Onsite or via Retrieval Services Queensland (RSQ) usually in conjunction with ENT. |
Non-critical child
| Reason for contact by clinician | Contact |
|---|---|
For specialist advice on the management, disposition and follow-up of the following stable children:
|
As per local practice. Options:
|
| For specialist advice on the management of a child with normal X-ray and persistent symptoms more than one week after a choking episode. | Onsite/local Paediatric Respiratory service else onsite/local ENT or Paediatric service as per local practices |
Inter-hospital transfers
| Do I need a critical transfer? |
|
| Request a non-critical inter-hospital transfer |
|
| Non-critical transfer forms |
|
Disposition
When to consider discharge from ED
Discharge may be considered for a child with a history of a choking episode who meets the following criteria:
- has normal physical and radiological findings
- tolerates feeding
- remains asymptomatic following a period of observation.
Caregivers should be advised to seek medical attention and inform the doctor of a previous choking episode should the following symptoms develop within a month:
- persistent cough
- fever
- noisy, fast or difficulty breathing or grunting
Provide the following prevention advice to all caregivers:
- hard and/ or round foods should not be offered to children younger than four years of age
- infants and young children should be fed when sitting upright and with adult supervision
- small objects including marbles, small balls, coins, button batteries and balloons should be kept out of reach of young children
- follow the age recommendations on toy packages
When to consider admission
As per consultation, a child may be admitted under a specialist service for ongoing management.
-
- Srivastava, G., (2010), ‘Airway Foreign Bodies in Children’. Clinical Pediatric Emergency Medicine, Vol. June 11(2) pp. 67-72
- ALSG APLS
- Rempe, B., Iskyan, K., Aloi, M. (2009), ‘An Evidence-Based Review of Pediatric Retained Foreign Bodies’. Pediatric Emergency Medicine Practice, Vol. Dec 6 (12)
- Heim, S.W., Maughan, K.L, (2007), ‘Foreign Bodies in the Ear, Nose, And Throat’. American Family Physician, Vol 76 pp.1185-9
- Cohen, S., Avital A., Godfrey, S., Gross, M., Kerem, E., Springer, C., (2009), ‘Suspected Foreign Body Inhalation in Children: What Are the Indications for Bronchoscopy?’, The Journal of Paediatrics, Vol. Aug 155(2) pp. 276-80
-
Document ID: CHQ-GDL-60020
Version number: 3.0
Supersedes: 2.0
Approval date: 01/03/2023
Effective date: 01/03/2023
Review date: 01/03/2025
Executive sponsor: Executive Director Medical Services
Author/custodian: Queensland Emergency Care Children Working Group
Applicable to: Queensland Health medical and nursing staff
Document source: Internal (QHEPS) + External
Authorisation: Executive Director Clinical Services
Keywords: Inhaled, foreign body, paediatric, emergency, guideline, children, 60020
Accreditation references: NSQHS Standards (1-8): 1, 3, 8
-
This guideline is intended as a guide and provided for information purposes only. View full disclaimer.
Last updated: October 2023