View resources
Key points
- Serious paediatric cervical spine injuries (CSI) following blunt trauma are uncommon and those that are unstable generally result from high force or high angular momentum or distraction.
- Within the subgroup of children with severe injury mechanisms, particularly those with altered conscious state, radiological signs of spinal injury may be subtle, and clearance may require clinical, radiological, and spinal expertise.
- Risk factors for CSI include high-risk motor vehicle accident (MVA), diving or other axial load, medical conditions predisposing to CSI, substantial torso injury, altered mental status, focal neurological deficit, neck pain and traumatic torticollis.
- Seatbelt-restrained infants who experience a sudden, massive deceleration are particularly at risk of CSI due to a proportionately heavy head and poor cervical musculature.
- Imaging is only recommended for children with risk factor/s identified on careful assessment.
- Soft collars are recommended. Hard collars are of no known benefit and potentially harmful.
- Seek senior emergency advice if symptoms persist, regardless of radiological findings.
- Suspect acute cervical facet joint dislocation in a patient who presents with history of a low velocity, high force injury with a combination of hyperflexion and loading e.g. rugby scrum collapse, abnormal focal neurology suggestive of cord injury, and normal conscious state.
- Seek urgent Orthopaedic advice (onsite or via Retrieval Services Queensland (RSQ) if suspect acute cervical facet joint dislocation or spinal cord injury.
Purpose
This document provides clinical guidance for all staff involved in the care and management of a child presenting to an Emergency Department (ED) in Queensland with a possible cervical spine injury following blunt trauma.
This guideline has been developed by senior ED clinicians and Paediatricians across Queensland, with input from Orthopaedic and Spinal surgeons, Queensland Children’s Hospital, Brisbane. It has been endorsed for statewide use by the Queensland Emergency Care of Children Working Group in partnership with the Queensland Emergency Department Strategic Advisory Panel and the Healthcare Improvement Unit, Clinical Excellence Queensland.
Introduction
Serious paediatric cervical spine injury following blunt trauma is rare, occurring in approximately 1% of all paediatric blunt trauma cases, with incidence ranging from 0.4% in the preschool population to 2.5% in the adolescent age group.1, 2 Of these injuries, the majority are stable injuries, while approximately 35% have varying degrees of instability requiring bracing or operative fixation.3
Severe cervical spine injuries generally occur from high-risk mechanisms and present with clinical red flags. Owing to the complexity of radiological interpretation and assessments of stability, and the large ‘denominator’ of children with blunt trauma, there is a critical need for stepwise risk stratification, so that greater expertise and imaging with higher radiation or more sophisticated modalities is reserved for higher-risk children and mechanisms.
The traditional cervical spine clearance algorithms (NEXUS and Canadian C-Spine Guidelines) have demonstrated significant value in assessing adult populations. However, the Canadian C-Spine guidelines have not been validated in children and the Viccellio analysis of the NEXUS rule in 3065 blunt trauma paediatric patients to age 18, included only 30 children with cervical spine injuries, and only 4 under 9 years of age. The PECARN multicentre case-control analysis of factors distinguishing 540 cervical spine injuries in children aged under 16 years, and subsequent prospective study of over 4091 children4 provides the most paediatric specific evidence available and forms the basis of this guideline. Results from a larger child specific PECARN prospective study are expected in the next year or so, and are expected to inform future guidelines. The Australia/NZ multicentre SONIC study (recruitment commenced in 2021) will in future provide better understanding of the use and value of these three risk factor sets in our local paediatric population. Meanwhile it is important to ensure a broad interpretation of their model and to be aware of other mechanisms known to be associated with spinal injury including falls, tumbling and trampolining.
A review of paediatric CSI cases at the two Queensland children’s hospitals during the six-year period of 2008-2013 identified 38 patients aged less than 16 years who sustained a severe spinal injury requiring neurosurgical input (fractures, dislocations, spinal cord injury or combination of these, with input being surgery, traction, brace or plaster fixation). Of these 38 patients, 18 were 8 years of age or younger, and all patients in this age group had occiput-C2 lesions. In patients aged 9-16 years of age, 8 out of 20 had low velocity “facet joint dislocation” type injury.5
Assessment
Emergency care should always involve a rapid primary survey with evaluation of (and immediate management of concerns with) airway, breathing, circulation and disability (ABCD) followed by a thorough secondary survey. Pay specific attention to the maintenance of neutral spine positioning.
Patients with suspected CSI or high risk traumatic injury transferred from other hospitals should have a full C-spine assessment undertaken on arrival in ED or ICU, in view of the high risk of subtle or occult injury.
History
History is critical in the risk assessment of paediatric patients with suspected CSI.
Questioning should include information on:
- mechanism of injury
- past medical history (see below for conditions that may predispose to CSI)
- symptoms post-incident including neurological symptoms, neck pain, ambulation and respiratory distress.
Conditions that may predispose to CSI
- Down syndrome (shallower facet joints and hypotonia causing increased risk of horizontal displacement)
- Klippel-Feil syndrome
- achondroplasia
- mucopolysaccharidosis
- Ehlers-Danlos syndrome
- Marfan syndrome
- osteogenesis imperfecta
- Larsen syndrome
- juvenile rheumatoid arthritis
- juvenile ankylosing spondylitis
- renal osteodystrophy
- rickets
- history of CSI or cervical spine surgery
- occult congenital deformity such as os odontoideum (a congenitally short odontoid peg limiting the effectiveness of the transverse ligament)
Examination
Do NOT reposition a conscious child with torticollis unless there are airway concerns. Seek urgent Spinal Fellow advice if an unstable fracture/dislocation severely compromising spinal canal diameter is identified on imaging.
Pain vs tenderness
A traumatic cervical spine injury like any other traumatic deformation causes the conscious infant, child or adolescent to be acutely aware of pain and dysfunction, and to protect the area with muscle spasm. The PECARN study found a complaint of neck pain to be a significant risk factor for CSI while midline “tenderness” was NOT associated with CSI. Asking children (where appropriate) where they are sore, and assessing posture, mobility and clinical responses can help differentiate pain from tenderness.
Active range of motion
An assessment of active range of motion is only recommended for patients with no pain, no abnormal neurology, and no altered conscious state as an indication for imaging. While active neck rotation to 45⁰ bilaterally is considered an appropriate range of motion in adults, asymmetrical or painful limitation of movement at 45-90⁰ may be significant in children.
Assessing infants and young children
Assessment of infants and young children presents a particular challenge for the clinician. While relevant history may be obtained from parents or other witnesses, subjective description of symptomatology is unreliable and difficult. History and objective examination findings must be synthesised to determine the need for investigations and/or observation.
In general, CSI in young children is very rare: a 10-year review of more than 12,000 cases of blunt trauma from 22 Trauma Registries in USA identified only 83 children aged up to 36 months with CSI. All children had at least one of the following features: MVA, GCS less than 14, GCS eye = 1, reduced neck mobility, or face or skull fractures.6
The radiation risk in this age-group is higher while the sensitivity of plain films for injury or instability is lower. Assessment of the young child and interpretation of the young child’s radiology may require a high degree of sophistication and experience.
Risk factors for significant CSI in children
- high-risk motor vehicle accident (MVA) includes head-on collision, rollover, ejection from vehicle, death in same crash, or speed in excess of 88km/hour
- axial load to the head e.g. diving, trampolining, falling from a height
- forced neck hyperflexion (low velocity, high force) e.g. rugby scrum collapse, clotheslining
- altered conscious state (GCS<15, AVPU <A, intoxicated, confused)
- traumatic torticollis (a preference for a rotated position and/or a decrease in cervical spine range of movement, difficulty moving the neck)
- respiratory symptoms (includes distress and decreased saturations)
- substantial torso injury (includes clavicles, abdomen, flanks, back, spine and pelvis)
- focal neurological deficit (paraesthesia, loss of sensation, motor weakness, or other e.g. priaprism)
- other specific features of spinal cord injury such as unexplained refractory hypotension
- neck pain (see pain vs tenderness section above)
Acute cervical facet joint dislocation
Patient (typically adolescent) presents with:
- history of a low velocity injury with hyperflexion or axial loading (e.g. rugby scrum collapse)
- abnormal focal neurology suggestive of cord injury
- normal conscious state.
The abnormality is readily apparent on plain films. Time to traction/reduction is critical.
Seek urgent orthopaedic advice (onsite or via RSQ) if suspect acute cervical facet joint dislocation or spinal cord injury.
Thoracolumbar spinal injury
Risk factors include:
- high velocity MVA particularly if sash or harness restraint devices have not been worn
- ejection from MVA
- high speed motor bike/bicycle collisions in which patient has gone over handlebars landing on head prior to impact
- multi-trauma victims with unclear mechanism of injury and altered conscious state
- abnormal focal neurology
- localised thoracolumbar pain
- spinal injury at other levels
Investigations
Imaging is associated with radiation risks (exact exposure dependent on the machine used and site-specific protocols) and interpretation of findings can be complex. Imaging based on risk approach is recommended. Analgesia and reassessment prior to immediate imaging may be an appropriate management strategy in some children.
The risks and benefits of each imaging modality needs to be carefully considered. While in adult populations CT is generally preferred where available, this is not routinely recommended in children due the increased risks associated with radiation and the potential need for sedation.
Imaging to identify CSI in children
Considerations for each imaging type are outlined below.
Plain films
- sensitivity estimated at 90% but may be as low as 75% in age 0-3 years with severe mechanisms, as distraction failure in the occiput-C2 region is not readily apparent on plain films
- 10-20% of radiation exposure when compared with CT scan
- three views (antero-posterior, lateral and odontoid peg) where technically feasible, increase the sensitivity to detect clinically-significant CSI compared to fewer views
- odontoid peg views are technically difficult (may be obscured by teeth or occiput)
- able to identify malalignment e.g. facet joint subluxation/dislocation in sagittal view and torticollis in coronal plain view
Of the 542 children with CSI in PECARN, 18 had no abnormality detected on plain films. However, all had at least one risk factor for CSI. The four who required operative stabilisation presented with abnormal focal neurology following a high-risk mechanism of injury (os odontoideum and fall/flip (n=2), atlanto-occipital dislocation from MVA (n=1) and unilateral facet fracture/dislocation (n=1) following a trampoline fall.7
CT scan
- gold standard for identifying bony injury
- sensitivity to detect significant CSI in children is not 100% as findings can be subtle (e.g. small avulsion demonstrated in a single slice of a CT series). Careful assessment of overall risk is important
- potential cancer risks exist from the ionising radiation:
- CT scans have been estimated to triple the risk of leukaemia and brain cancer – 10 years after the first CT scan in children less than 10 years of age, one excess leukaemia case and one excess brain tumour case per 10, 000 head CT scans is estimated to occur.8
- extrapolation of physical data for radiation exposure during imaging on models at QCH demonstrated that the risks are greater in younger children and females, and that the radiation in a cervical spine CT series has an effective thyroid radiation dose approximately 10 times that of the 3-plain film series.9
MRI scan
- superior sensitivity for identifying ligamentous and soft tissue injury, particularly infants with high energy mechanisms10
MR angiography
- can identify vertebral artery injuries that may be associated with CSI
- consider in the following children:
- high cervical spine injuries
- fractures involving transverse foramen
- neurological signs suggestive of vertebral artery insufficiency including vertigo, mental state changes or unilateral weakness
Decision making should include radiological and spinal teams in consideration of the risks of imaging and of potential treatment in the clinical context. In practice anticoagulation would rarely occur due to the severity of associated blunt trauma.
In view of the above considerations and the availability of local resources, general recommendations are outlined below.
Imaging to identify CSI in children
| Imaging type | Utility |
|---|---|
| Plain films |
|
| CT scan |
|
| MRI scan |
|
Seek senior emergency advice on choice of imaging for a child with risk factor/s for CSI.
Management
Refer to flowchart [PDF 738.83 KB] for a summary of the emergency management of a child following a CSI.
Spinal immobilisation in children
Immobilisation and spinal precautions are recommended for all children with risk factor/s for CSI until assessment has taken place and CSI has been excluded. Patients at risk of thoracolumbar spinal injury should be kept flat, with neutral positioning of the entire spine and log-rolling.
Infants may be brought into ED having been immobilised in a whole-body vacuum splint. These splints facilitate safe transport from the pre-hospital setting, however must be removed to allow full assessment. This involves deflating the splint, applying a cut-down soft collar if not already applied and log roll for any transfers.
The Queensland Ambulance Service, Princess Alexandra Hospital (PAH) Spinal Injuries Unit and Queensland Children’s Hospital recommend the MOR approach which involves LESS discomfort and risk of pressure complications (the change from stiff to soft collars) but MORE attention to addressing Moments of Risk (MOR) in the smaller number of higher-risk patients.
MOR approach to immobilisation
Specific aspects of the MOR approach include:
- soft neck collars
- thoracic elevation devices (TEDs) in children aged less than 8 years
- lateral sandbags in unconscious patients
- careful attention to neutral handling and positioning at moments of risk
| Specific consideration in children | Strategies to promote neutral positioning |
|---|---|
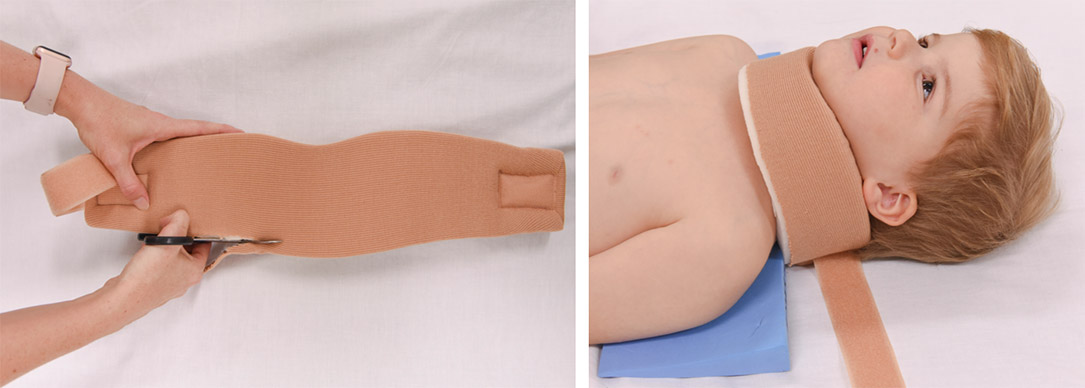
| Short submental distance. | Collar needs to be snugly fitted to reduce risk of hyperflexion due to chin slipping (see image below). |
| Poor tolerance for immobilisation which can lead to agitation. | See table below. |
| Natural desire to look around. | Position parents at head of bed to avoid hyperflexion. |
| Cobb angle (the difference in inclination of lines drawn parallel to inferior endplates of C2 and C6) is in the flexed range in a younger child when lying flat. | Position a TED high under the neck when immobilising children less than 8 years of age (see image below). |

Neck collars
As with all mechanical trauma to the skeleton, deformations causing spinal cord injury or ischemia occur at the time of the initial massive angulating / displacing forces and are unlikely to be reproduced during normal handling. No orthopaedic immobilisation device can prevent angulation during transfers when high level instability is present, and the differences in angulation between one-piece, two-piece and soft devices with cervical spine precautions during handling is small.11 Standard cervical collars cannot prevent anteropulsion of horizontally unstable injuries, or the risks associated with atlanto-occipital instability.
Soft collars should be used to immobilise the cervical spine. If needed, soft collars can be cut along the lower edge to ensure a snug fit under the chin.
Hard collars are not recommended. There is no evidence of efficacy.10 Potential harm associated with use include raised intracranial pressure, respiratory disturbance, patient agitation, and soft tissue ulceration.12
Thoracic elevation device (TED)
TEDs are foam wedges designed to improve spinal and airway positioning in children.13
TEDs should be used when immobilising a child aged less than 8 years.
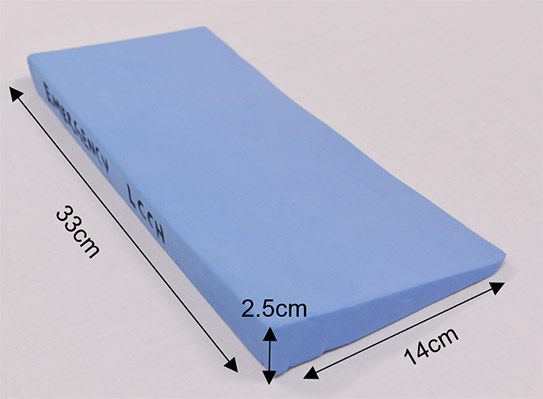
- The recommended dimensions are 33cm W * 14cm L * 2.5 cm H.
- TEDs can be cleaned between patients to allow reuse if covered in a nonporous material (such as plastic).
- They can be custom made from foam supply companies or are commercially available from medical imaging companies
Moments of risk
| Moment of risk | Strategies to protect cervical spine |
|---|---|
| Trolley transfers and log roll |
|
| Pain/agitation |
|
| Vomiting |
|
| Voiding |
|
| Imaging |
Attendant to:
|
| Intubation |
|
Child with no risk factors or pain as only risk factor for CSI
- C-spine imaging is not required initially
- explain to patient and guardian that the risk of a clinically significant C-spine injury is very low
- if required administer Ibuprofen 10mg/kg + Paracetamol 15mg/kg if no contraindications
- prop patient up
- consider soft collar
- observe for 30-60 minutes if neck pain and/or limited range of motion
- consider further imaging if neck pain and/or limited range of motion persists on re-assessment
Clinical clearance of CSI
While evidence is limited, CSI can be clinically excluded in a child with no risk factors (including pain) identified on careful assessment (history and examination).
Consider seeking senior emergency advice as per local practice for child with persistent pain.
Child with at least one risk factor/s for CSI other than pain
Seek urgent orthopaedic advice (onsite or via Retrieval Services Queensland (RSQ)) if suspect acute cervical facet joint dislocation or spinal cord injury.
Unstable child
Seek immediate onsite assistance (anaesthetics/critical care/ENT) as per local practice to manage airway.
Seek urgent paediatric critical care advice (onsite or via RSQ) for unstable child.
Manage ABCD as per APLS.
Immobilise with soft collar. If aged less than eight years use a thoracic elevation device (refer to Immobilisation and spinal precautions section below).
Consider the possibility of neurogenic shock in any hypotensive trauma patient if hypotension persists despite fluid resuscitation and without accompanying tachycardia.
Trauma patients with altered conscious state must be considered at high risk of unstable cervical spine injury +/- spinal cord injury. Recommended actions include:
- where possible, document all four limb movements/sensorimotor responses prior to paralysis for ventilation
- exercise care when interpreting cervical spine imaging as even CT evaluation may fail to identify ligamentous instability
- monitor mean blood pressure with a rigorous and interdisciplinary evaluation of hypotension
- consider neurogenic shock (characterised by persistent and refractory hypotension without accompanying tachycardia) while simultaneously actively pursuing other traumatic causes of haemorrhagic shock
- consider cerebral and spinal perfusion pressure to avoid secondary hypoperfusion injury. Inotropic support may be required (on paediatric critical care advice).
Stable child
- C-spine imaging is recommended (refer to Investigations)
- administer Ibuprofen 10mg/kg + Paracetamol 15mg/kg if no contraindications as required
- reassess child (including active range of motion) if no abnormality is detected on imaging
Prompt referral to local orthopaedic team is required for child with abnormality detected on imaging.
Seek senior emergency/orthopaedic advice as per local practice for a child with no abnormality detected but ANY of the following:
- altered mental status
- focal neurological deficit
- persistent neck pain
- persistent torticollis
CSI clearance
CSI can be excluded in a child presenting with risk factor/s with:
- no abnormality detected on imaging
AND
- no persistent symptoms during observation period including:
- altered mental status
- focal neurological deficit
- neck pain
- torticollis
Following CSI clearance:
- explain to patient and guardian that the risk of a clinically significant C-spine injury is very low
- remove splinting and cease spinal precautions
- recommend sitting posture and encourage gradual mobilisation
In practice many of these children are slow to mobilise particularly if they have been transported with spinal injury precautions.
Escalation and advice outside of ED
Clinicians can contact the services outlined below to escalate the care of a paediatric patient as per local practices.
Child who is unstable or requiring time-critical care
Maintain a high index of suspicion for acute cervical spine instability in a seat-belt restrained infant involved in a high force rapid deceleration injury, even if initial imaging appears normal.
Suspect acute cervical facet joint dislocation in the older, conscious child who presents with the following:
- history of a hyperflexion and loading injury e.g. rugby scrum collapse
- abnormal focal neurology suggestive of cord injury
Time-critical care is required in child with:
- acute cervical facet joint dislocation- aim for reduction within four hours
- spinal cord injury
| Service | Reason for contact | Who to contact |
|---|---|---|
| Orthopaedics | First point of call for child with:
| Onsite or via RSQ (access via QH intranet) or on 1300 799 127:
Notify early of children potentially requiring transfer. |
| Spinal | For review of PACS images in concerning cases | Contact usually via Orthopaedics else via Children’s Hospital experts via Children’s Advice and Transport Coordination Hub (CATCH) on 13 CATCH (13 22 82) (24-hour service) |
| For immediate onsite assistance including airway management | For onsite help with the management of airway, including intubation and ventilation. | The most senior resources available onsite at the time as per local practices. Options may include:
|
Stable child not requiring time-critical care
| Reason for contact by clinician | Contact |
|---|---|
For specialist advice on the management, disposition and follow-up of the following children:
| Onsite/local orthopaedic service as per local practice. |
Inter-hospital transfers
| Do I need a critical transfer? |
|
| Request a non-critical inter-hospital transfer |
|
| Non-critical transfer forms |
|
Disposition
When to consider discharge from ED
Consider discharge for patients in whom CSI has been excluded providing there are no other concerns.
On discharge parents/caregivers should receive appropriate advice regarding analgesia and expected recovery (which may take weeks).
Follow-up
- with GP within a week.
Patients who have been assessed by the orthopaedic or spinal team may be discharged home for early outpatient review, with or without ongoing immobilisation, at the subspecialty team’s discretion.
When to consider admission
Patients with confirmed CSI, altered conscious state or focal neurological deficits require admission with spinal immobilisation and spinal precautions until function can be adequately assessed. Clearance of these children is a multidisciplinary responsibility requiring input from PICU, radiology, and spinal services. Handling to maintain neutral positioning and minimise pressure effects can be challenging.
Children in whom there are persistent symptoms such as pain or torticollis despite normal initial imaging may require a period of admission at the discretion of the treating specialist team.
-
- Mohseni, S., Talving, P., Branco, B. C., Chan, l. S., Lustenberger, T., Inaba, K., Bass, M. & Demetriades, D. 2011. Effect of age on cervical spine injury in pediatric population: a National Trauma Data Bank review. Journal Of Pediatric Surgery, 46, 1771-1776.
- Shin, J. I., Lee, N. J. & Cho, S. K. 2016. Pediatric Cervical Spine and Spinal Cord Injury: A National Database Study. SPINE, 41, 283–29
- Leonard, J.C., Kuppermann, N., Olsen, C., Babcock-Cimpello, L., Brown, K., Mahajam, P., Adelgais, K.M., Anders, J., Borgialli, D., Donoghue, A., Hoyle, J.D., Kim, E., Leonard, J.R., Lillis, K.A., Nigrovic, L.E., Powell, E.C., Rebella, G., Reeves, S.D., Rogers, A.J., Stankovic, C., Teshone, G., Jaffe, D.M. 2011. Factors Associated with Cervical Spine Injury in Children After Blunt Trauma. Annals of Emergency Medicine, 58, 145-155
- Leonard, J.C., Browne, L.R., Ahmad, F.A., Schwartz, H., Wallendorf, M., Leonard, J.R., Lerner, B., Kuppermann, N. 2019. Cervical Spine Injury Risk Factors in Children with Blunt Trauma. Pediatrics, 144 (1): e20183221
- Purushothaman, B., Rasmussen, K., Williams, J., Phillips, N., Brady, R., Duckworth, G., Walsh, M., Labrom, R. & Askin, G. 2015. Utility of plain xrays in identification of severe paediatric spinal injury in Australia Spine Society of Australasia.
- Pieretti-Vanmarcke, C. R., Velmahos, L. G., Nance, A. M., Islam, W. S., Falcone, L. R., Wales, A. P., Brown, O. R., Gaines, W. B., Mckenna, R. C., Moore, R. F., Goslar, L. P., Inaba, S. K., Barmparas, A. G., Scaife, K. E., Metzger, D. R., Brockmeyer, P. D., Upperman, F. X. J., Estrada, H. J., Lanning, W. D., Rasmussen, D. S., Danielson, D. P., Hirsh, F. M., Consani, D. H., Stylianos, E. S., Pineda, S. C., Norwood, A. S., Bruch, M. S., Drongowski, T. R., Barraco, T. R., Pasquale, T. M., Hussain, T. F., Hirsch, T. E., Mcneely, T. P., Fallat, T. M., Foley, T. D., Iocono, T. J., Bennett, T. H., Waxman, T. K., Kam, T. K., Bakhos, T. L., Petrovick, T. L., Chang, T. Y. & Masiakos, T. P. 2009. Clinical Clearance of the Cervical Spine in Blunt Trauma Patients Younger Than 3 Years: A Multi-Center Study of the American Association for the Surgery of Trauma. The Journal of Trauma: Injury, Infection, and Critical Care, 67, 543-550.
- Nigrovic L, R. A., Adelgais K, Olsen C, Leonard JR, Jaffe D, Leonard JC 2012. Utility of Plain Radiographs in Detecting Traumatic Injuries of the Cervical Spine in Children. Pediatric Emergency Care, 28, 426-432.
- Pearce, M. S., Salotti, J. A., Little, M. P., Mchugh, K., Lee, C., Kim, K. P., Howe, N. L., Ronckers, C. M., Rajaraman, P., Craft, S. A. W., Parker, L. & González, A. B. D. 2012. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. The Lancet, 380, 499-505.
- Ryan, E. 2018. Effective Radiation Doses for Cervical Spine Imaging, LCCH. LCCH.
- Henry, M., Riesenburger, R. I., Kryzanski, J., Jea, A. & Hwang, S. W. 2013. A retrospective comparison of CT and MRI in detecting pediatric cervical spine injury. Child’s Nervous System: Chns: Official Journal Of The International Society For Pediatric Neurosurgery.
- Horodyski, M., Dipaola, C., Conrad, B. & Rechtine, G. 2011. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J Emerg Med, 41, 513-518.
- Kwan, I., Bunn, F. & Roberts, I. 2009. Spinal immobilisation for trauma patients. Cochrane Database Of Systematic Reviews (Online).
- Pandie Z, S. M., Lamont T, Walsh M, Phillips M, Page C 2009. Achieving a neutral cervical spine position in suspected spinal cord injury in children: analysing the use of a thoracic elevation device for imaging the cervical spine in paediatric patients. Emerg Med J, 2010, 573-576.
-
Document ID: CHQ-GDL-60025
Version number: 2.0
Supersedes: 1.0
Approval date: 13/06/2022
Effective date: 13/06/2022
Review date: 13/06/2026
Executive sponsor: Executive Director Medical Services
Author/custodian: Queensland Emergency Care Children Working Group
Applicable to: Queensland Health medical and nursing staff
Document source: Internal (QHEPS) + External
Authorisation: Executive Director Clinical Services
Keywords: Paediatric, emergency, guideline, cervical spine, blunt trauma, CSI, spinal injury, 60025
Accreditation references: NSQHS Standards (1-8): 1, 8
-
This guideline is intended as a guide and provided for information purposes only. View full disclaimer.
Last updated: March 2024