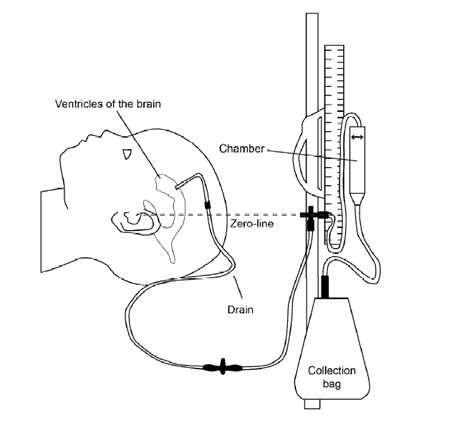
An external ventricular drain (EVD) is a temporary method that uses gravity to drain cerebrospinal fluid (CSF) out of compartments in the brain, called ventricles, via a thin tube that goes out of the head into a chamber and bag. The tube is inserted into the brain while your child is under a general anaesthetic in the operating theatre. The tube is stitched in and the insertion site is covered with a dressing.
What is cerebrospinal fluid?
CSF is a fluid that is continuously made in the ventricles in the brain. It flows through the brain and spinal cord, before later being reabsorbed. Cerebrospinal fluid provides cushioning and nutrients to the brain and spinal cord.
Why is an EVD needed?
Sometimes infection, injury or other conditions may cause either too much CSF to be made, not enough to be reabsorbed, or the flow of CSF to become blocked. The CSF builds up creating pressure within the brain. An EVD will relieve the pressure by draining off some of the CSF. The amount drained is variable and depends on several factors including height of the chamber in relation to the ventricles in the brain. The drain will be adjusted every time your child changes position. This will help reduce the problems associated with either over drainage or under drainage of CSF.
What happens after the surgery?
Your child will be closely monitored by their allocated nurse. In some cases, the nurse will remain in the room at all times to make regular neurological observations.
Your child’s nurse will be watching to see if your child:
- seems irritable, confused, disorientated, or just not their usual self
- seems more sleepy than usual
- says they have a headache
- vomits or complains that they feel sick
- says that they have double vision or blurry vision
- has fluid leaking from the head or tubing
Your nurse will clamp the EVD before your child sits up, lies down or is picked up. After the height of the EVD is adjusted, then the nurse will open the clamps.
Your nurse will empty the chamber hourly while keeping the system closed to reduce the risk of infection.
The amount of CSF drainage will be recorded. Cerebrospinal fluid specimens will be taken for testing from the EVD when requested by doctors.
What do I need to do?
Tell your child’s nurse immediately if your child changes position (e.g. sits up or lies down) or before you pick your child up. Under no circumstances should anyone except your nurse or doctor touch the EVD. Avoid excessive flexion and extension of your child’s neck, as this can cause disruption in the flowing of fluid and increase pressure. Please also help prevent infection by ensuring you and all visitors regularly wash your hands or use hand gel.
Daily activities
You can help your child with many of their usual daily activities, with assistance from your child’s nurse. Your child may be able to sit on the edge of the bed, or go for a short walk, with the assistance from your child’s nurse or physiotherapist.
Will my child be in pain?
An EVD should not cause pain however Paracetamol will be available as needed, as well as additional pain relief, depending on your child’s condition.
When will the EVD be removed?
The length of time an EVD is needed varies. Your child’s neurosurgeon will discuss with you when it may be removed. The EVD will be removed by the doctor either on the ward, or in the operating theatre if further surgery is required. After the EVD is removed a permanent method of draining CSF is sometimes needed. This is known as a shunt. If your child is likely to need a shunt, the neurosurgeon will discuss this with you.
Breastfeeding
You can still breastfeed your child when they have an EVD. Please let your child’s nurse know if you would like to continue to do so, and they can assist you with positioning techniques.
When to seek help
See your GP if your child has any common symptoms.
In an emergency, call Triple Zero (000) and ask for an ambulance.
If you're not sure whether to go to an emergency department, call 13 HEALTH (13 43 25 84) and speak to a registered nurse.
Developed by the Department of Neurosciences, Queensland Children’s Hospital. We acknowledge the input of consumers and carers.
Resource ID: FS142. Reviewed: January 2016.
Disclaimer: This information has been produced by healthcare professionals as a guideline only and is intended to support, not replace, discussion with your child’s doctor or healthcare professionals. Information is updated regularly, so please check you are referring to the most recent version. Seek medical advice, as appropriate, for concerns regarding your child’s health.
Last updated: October 2023